I see it’s been about 5 months since my last update. What’d I miss?
Not COVID-19. I caught it again in late July, with an additional dollop of rebound COVID-19 about a week after finishing Paxlovid for the initial infection. Compared to my first go round in August, 2022, this second round of COVID-19 had more chills, fatigue, a bit less coryza (sneezing, runny nose), but still with cough.
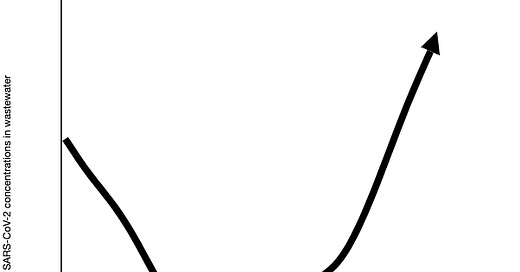
It seems I was in the vanguard this time. Wastewater data has shown increasing viral load, although, not spiking as quickly as we have found in other surges of activity. We are seeing more people getting COVID-19 —again; and some for their very first time.
And now new vaccines are rolling out, around the same time as influenza vaccination. In fact, you can get both at the same time! These vaccines are directed against a variant (XBB.1.15) that was dominant earlier this year. Of course, new variants have emerged, but the vaccine still looks effective against them.
So, should you get the vaccine? And if so, when? While I get these questions a lot, the answer is relatively straight forward—yes, if you are over 6 months of age, and as soon as you can, if you haven’t been vaccinated in the last two months. If you have recently had COVID-19, you could wait a bit longer.
But, there are always nuances. The CDC has a list of FAQs, that may be helpful.
Of course, the ideal time to get a vaccine is 2 to 4 weeks before you are exposed to a pathogen, as that is the amount of time after vaccination for peak antibody formation. However, since we never know when that exposure will be, it’s usually best to get vaccinated when you can.
What about if I had side effects after previous vaccination? Many people will have some vaccine-related response, such as pain around injection site, or muscle aches. The worrisome side effect of myocarditis (heart muscle inflammation) was seen in some young men with the mRNA vaccines in the past. It was not felt to be life threatening. Getting COVID-19 is more likely to cause myocarditis than the vaccine itself. If still concerned, then maybe the Novavax vaccine would be for you. However, we don’t know when that will be released.
What if I recently had COVID-19? Nobody knows the absolute right answer. We do know that there is some protection when recovering from infection, but that the protection will diminish over time. I plan to wait until Oct/Nov to get my booster, as I recovered in early August.
While getting vaccinated against COVID-19 and influenza is a “no-brainer” for most folks, the calculus around masking remains complicated. Who should mask, when should I mask, and does it even make a difference?
First of all, hopefully no one is using a cloth mask anymore. They don’t really protect you from others, and they don’t protect others from you very well. Are they better than nothing? Probably, but not by much.
A procedure mask that does not filter air is good for protecting others from you (“source control”), but really only make a difference when everyone uses them. We found these helpful in healthcare settings when everybody was wearing them. Back when we had Universal Masking (everybody masking), the only outbreaks we saw in healthcare workers was in break rooms—you can’t wear a mask efficiently when you’re eating and drinking. Lately, as masks are largely gone in healthcare settings, we are starting to see outbreaks on work units not associated with breakrooms. These procedure masks provide a bare smidgeon of protection for the wearer—again, better than nothing when it comes to COVID-19. They work better for other infections, such as influenza.
Well-fitted N95/KN95 provide the best protection against COVID-19 for the wearer. Again, they must be worn correctly and at almost all times when exposed. Remember, transmission is a numbers game, not an absolute or all-or-none process. The more you wear a mask correctly, the less likely you are to catch something.
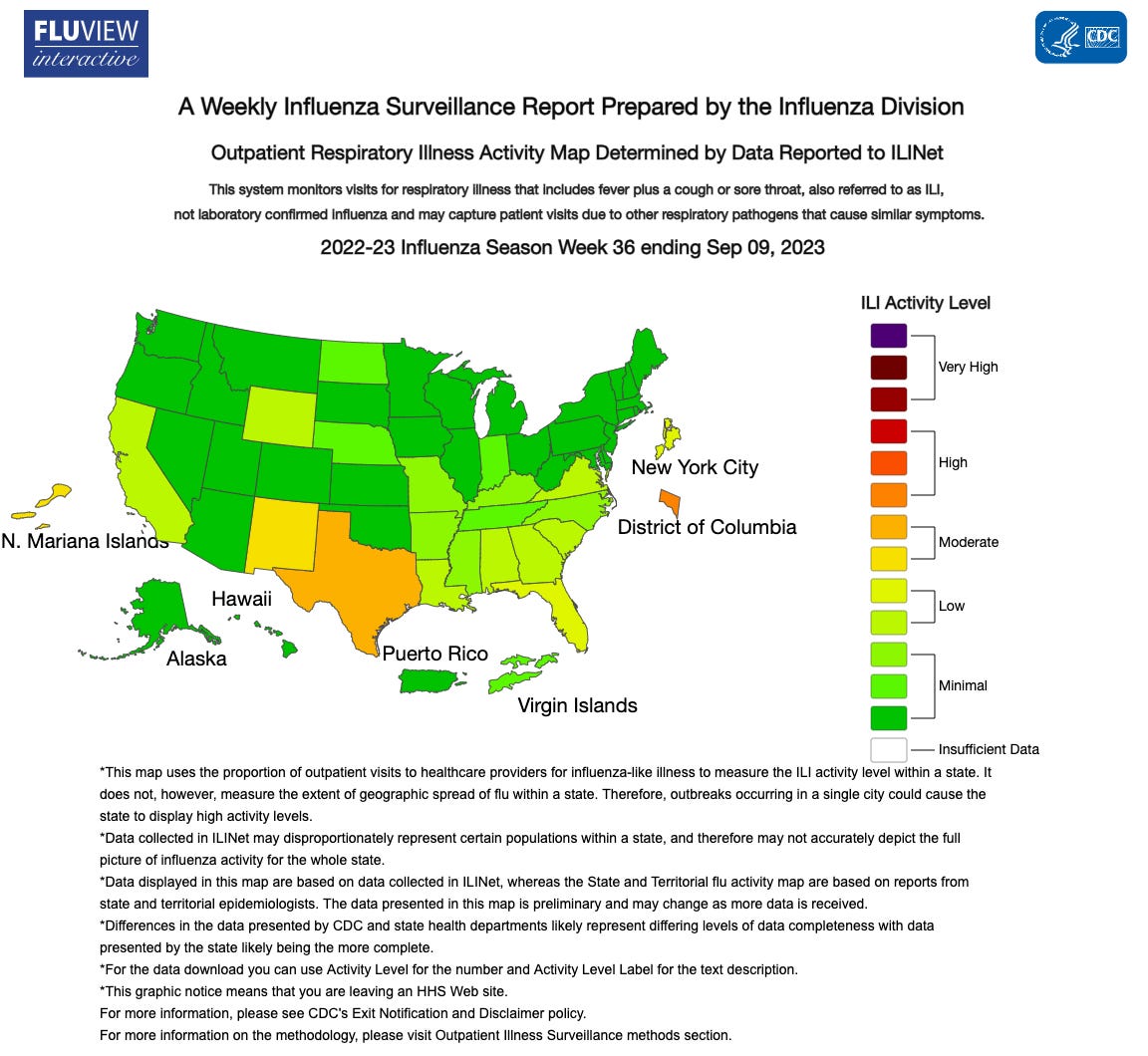
I’ll be wearing a procedure mask most of the time around patients—and all the time around vulnerable patients. I probably won’t be wearing a mask in public, at least not yet. But I’ll be keeping an eye on Influenza Like Illness in my state!
Be well!





What are the odds of a healthy child dying of Covid?