In my previous post, I discussed immunizations available for COVID-19 that are passive immunizations—giving antibodies from an external source such as a recovered patient or a laboratory. The principal shortcoming of passive immunizations is that they are time limited—they fade over weeks or months.
The real excitement for COVID-19 is almost here—active immunizations, also called vaccines.
A vaccine is an immunization that provokes the recipient’s immune system to defend against—something. Usually a germ, or maybe just part of a germ, such as a protein, or antigen. While all vaccinations are immunizations, not all immunizations are vaccinations. The great benefit of vaccinations over passive immunizations is that the protection is generally much longer lived—for months, years or even decades. The advantages of vaccines over natural infection (that is, catching the disease) is that you should get less sick, and be less likely to die or have severe complications, having received the vaccine.
I refer the interested reader to the history of vaccines at historyofvaccines.org The modern era of vaccines dates to 1796 and an English physician named Edward Jenner, who inoculated cowpox virus from a milkmaid to an 8 year old boy (no IRB needed), as a method to protect from smallpox.
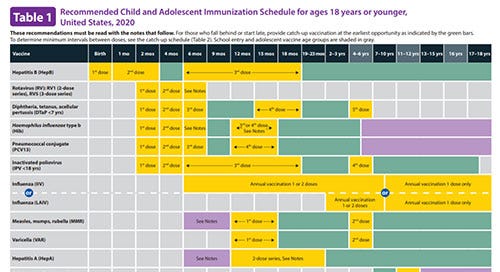
When I was a young internal medicine-pediatrics physician in training in the 1980’s, I could memorize the still short table of vaccines. Now there are so many, it is another reason to rely on the electronic health record to help us.
Image from CDC.gov
The New York Times is tracking 78 vaccines in various stages of development. The leading candidates are from Pfizer/BioNTech and Moderna. Both of these are vaccines that are truly novel in approach. Before this year, vaccines were typically either modified germs (alive or dead), such as influenza, measles, chickenpox—or were parts of germs, such as antigens (proteins). These modified germs or antigens would provoke the immune system to create antibodies, and sometimes other immune responses, to combat some future exposure to the infection targeted by the vaccine.
The Pfizer/BioNTech and Moderna vaccines do not contain ANY part of the germs at all. Instead, they contain messenger ribonucleic acid (mRNA). mRNA is a typically short lived form of RNA that instructs a cellular structure called a ribosome to create an amino acid sequence that then becomes a protein.
Image from nih.gov
These mRNA sequences have been designed to create a protein that is the spike protein of the SARS=CoV-2 (COVID-19) virus. People injected with this vaccine will have their own cells creating the protein, then their own immune system reacting to the protein, which then provides protection to the virus. These vaccines need to be kept extremely cold before being thawed out for administration.
These vaccines are a two injection sequence, several weeks apart.
The data from these studies in tens of thousands of volunteers indicate that protection is quite high (greater than 90 percent) during the study period. Severe adverse reactions that would require hospitalization are extremely low. Most common reactions are temporary soreness at injection site and some short-lived flu-like symptoms. These reactions indicate that the immune system is reacting to the vaccine, and should not be construed as vaccine failure.
The other vaccine that is coming up fast is from AstraZeneca and Oxford University. This vaccine uses a virus called adenovirus that has been modified to produce the COVID-19 spike protein. This vaccine has several advantages over the mRNA vaccines, including cheaper production and easier storage and distribution. Safety and effectiveness are still being assessed, but appear to be similar to the mRNA vaccines. Because this is a live virus vaccine, it may produce more side effects.
It is expected next week (Dec 8-10, 2020) that the FDA will be reviewing at least the Pfizer/BioNTech and Moderna vaccines for approval for distrubution. The British equivalent of the FDA has already approved the Pfizer/BioNTech vaccine.
These are the most common questions I am getting about the upcoming COVID-19 vaccines:
Which vaccination are you going to get?
I will take whichever one is available soonest. The COVID-19 pandemic is an immediate emergency, and there is no time to spare to get the vaccine.
When can I get my vaccination?
It is expected that the priority recipients of the vaccine will be healthcare workers, especially those taking care of the sickest patients such as in ERs and ICUs, and also patients and staff in long term care facilities (LTCFs). There has been some debate about how effective the vaccines are expected to be in the advanced elderly or very sick people who live in LTCFs. Fortunately, older patients were included in the trials, and appear to have some protection as well, at least based on early reports.
New York Times has created a calculator for determining place in line for receiving vaccine here.
What if I have already had COVID-19—should I still receive the vaccination?
We still do not know if having already had and recovered from COVID-19 means you should not get an immunization. Priority will probably be given to those who have never had the infection—hopefully the CDC will provide guidance.
I have heard that I can still get COVID-19 even if I get the vaccination.
This is true—but in people who received the vaccine, if they got the infection, it was generally less severe. We also don’t know whether if people who get the vaccine are also less likely to transmit the infection. The studies were designed to show that people who received the vaccine were less likely to get sick.
How long will the protection last?
Another unknown in a process borne of a crisis. We don’t know how long protection will last, and whether boosters will be needed every year (like influenza vaccines), every few years (like many vaccines) or never.
Will the vaccine make me sick?
It is expected that there will be some reaction to the vaccine. This is not vaccine failure. This means your immune system is working. Even if you have no reaction, likely you will have some immune response.
If I get the vaccine, does that mean I don’t need to wear a mask? Or use personal protection equipment (PPE) at work?
Among the questions that still need answers are whether people who received the vaccine can still spread the infection to others. For that reason, I will still wear a mask in public, and use PPE at work; and will do so until there is an “All clear” signal from public health authorities. On the other hand, I will have increased confidence that I am less likely to get sick, should I be exposed to the virus.
If you have more questions, please submit in the comments, and I will try to respond as time permits.
I hope all the front line workers and most vulnerable patients will receive the first vaccine dose by the end of the month.






nicely done.
Hello, Peter --Thank you for this, very helpful. I am at North Memorial now. Do you have any advice for vaccination of a group of doctors? Will we need to plan on possibly missing a day or two of work, should side effects occur? (As they side effects may include symptoms that would otherwise be suspicious for the infection.)