Since my last post, attention has turned to variants of SARS-CoV-2 (the virus that causes COVID-19 disease) that appears substantially more infectious than the previously predominant strain. What’s going on?
As an infectious disease specialist, I live with evolution and natural/unnatural selection everyday. Every time I treat a patient with a drug resistant organism, chances are good that the resistance developed as a consequence of some previous antibiotic exposure—although some germs are intrinsically resistant to some antibiotics. The development of resistance can be due to several reasons, but very often it is due to a mutation in the genetic code of the bacteria.
Mutations are changes that occur in the genetic code of all organisms that reproduce with either DNA (deoxyribonucleic acid) or RNA (ribonucleic acid). Almost all organisms have DNA, but viruses are different. They can have RNA or DNA as their genetic code. The genetic code is used to make proteins that are then used by the organisms in some way, either as structure or possibly enzymatic processing.
Some mutations can occur spontaneously; others can occur with help, such as exposure to chemicals (like in cigarette smoke) or from ionizing radiation, including X-rays and sun exposure. Many skin cancers are related to the natural ionizing radiation in sunlight. This is why dermatologists (and your parents) recommend sunscreen!
The faster a virus reproduces, the faster the chance for a mutation to occur. RNA viruses tend to develop mutations much faster than their hosts—about 1 million times faster—but it is not very fast—estimated to be on the order of one or two per month in a genome (total sequence of code) of 30,000+ units called nucleotides (a nucleotide refers to the specific type of building block of RNA—adenine, cytosine, guanine or uracil). In case you were wondering, humans have average of 100 to 200 genetic mutations per person. Our genome has 3 billion base pairs; each pair of nucleotides.
Many mutations go nowhere. Either they don’t cause a significant change in the protein that is coded by the sequence, or the change is so small that there is no functional difference in the protein. Sometimes the mutation may be lethal—it leads to a nonfunctioning protein, and the organism cannot function and dies, taking the lethal mutation with it.
But every now and then, a mutation may make a significant change in the function of the virus. If this change is not lethal, it can confer a competitive advantage of the virus. This competition between organisms that start with the same genetic code, but then develop a new functional mutation, is the basis of evolution. In viruses with new mutations, we call these variants. Technology has accelerated so that the whole genome of viruses can be determined quickly—we call this whole genome sequencing (WGS). This can be done in one to two hours in the laboratory.
The ultimate goal of life, at the genetic level, is to reproduce. One can question whether viruses count as life—they are really cellular parasites that lack the ability to live on their own. Viruses work by taking over the machinery of cells to recreate new viral particles. They cannot reproduce without other cells. For the sake of argument, let’s consider viruses “alive”.
Every time a mutation occurs, and is functional, this is called a variant. Many variants of COVID-19 have been described since the start of the pandemic. In the competition between new variants, what wins is fitness.

Viral fitness refers to the ability of a virus to spread and reproduce. The fitter the virus, the more widely it spreads. A highly lethal virus may not be fit. A dead host of a respiratory virus is not capable of transmitting disease. (Different story with Ebola, where even dead hosts can harbor live virus in tissue that can then infect others.)
COVID-19 has several characteristics that make it very fit:
there are many people who can spread the virus without having any symptoms
most cases are mild
even in people who get sick, they often can spread the disease before they have any symptoms
SARS-CoV-2 can live in both the upper and lower respiratory tract
Factors that would increase fitness (ability to spread and reproduce) in variants would be:
higher rates of replication
mutations that cause the virus to evade—or escape—from immune system or medications
An escape mutation is any mutation that would allow a new variant to evade, or escape, some controlling characteristic of the host. This could be host immunity from antibodies, either from vaccine or recovered from infection, or from some pharmaceutical control (which is what we call drug resistance).
Several variants have gained attention:
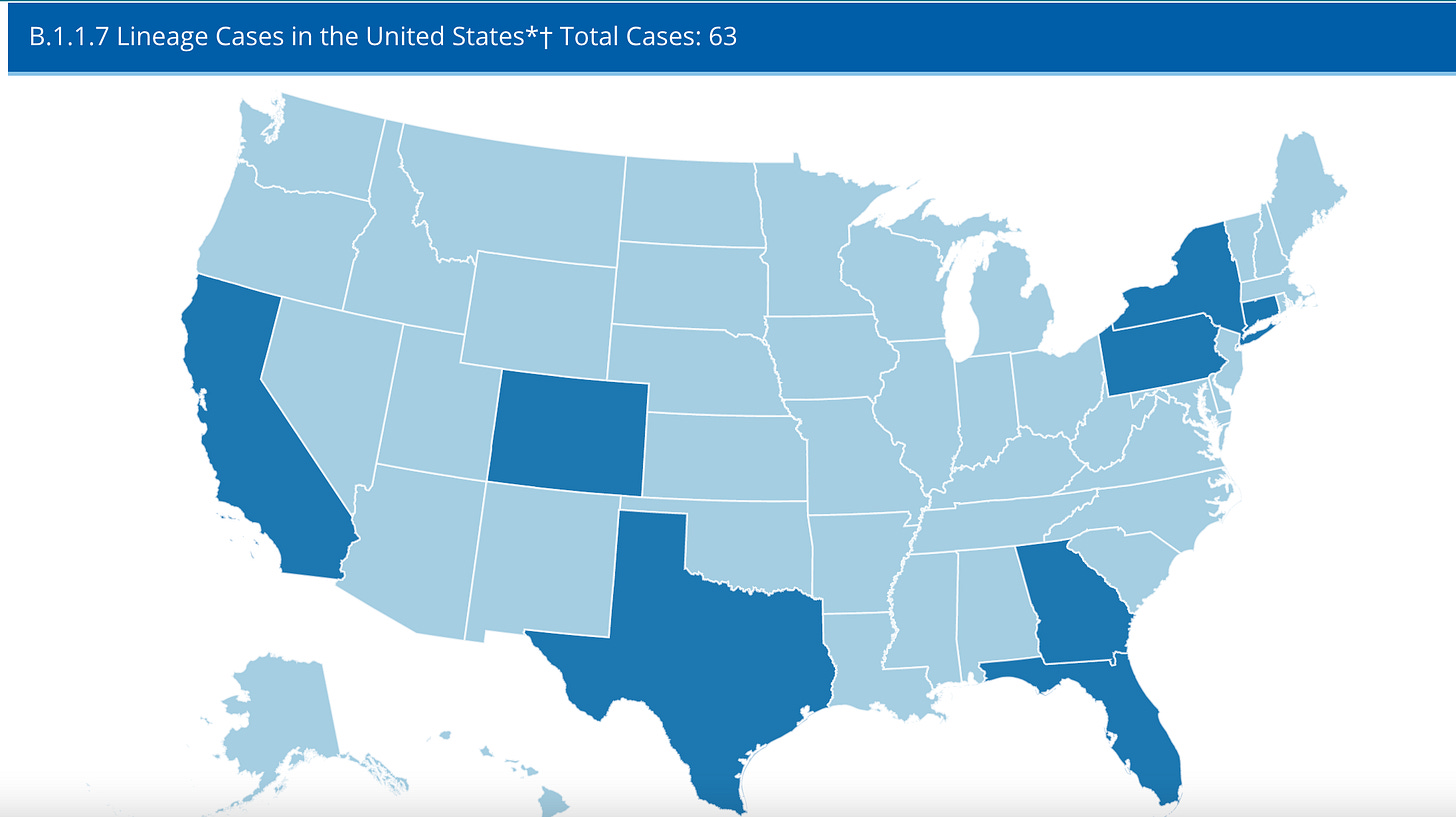
B.1.1.7 lineage variant in the UK has been associated with increased transmissibility, but not increased lethality. This increases fitness, displacing other previous variants or strains of virus. This new variant has been found in several US states, including Minnesota
B.1.35, also called E484K, lineage in South Africa shares some of the mutations as the UK variant, but is not the same. It, too, has increased transmissibility. Reports vary as to whether this strain is either more lethal or resistant to established immunity.
While so far these new variants do not seem to have increased lethality, which would harm viral fitness, they appear to be more transmissible, thereby increasing fitness.
The fear among epidemiologists is that given sufficient time, escape mutations may emerge that evade immunity, either from previous infection, or from vaccination.
The natural end state of SARS-CoV-2 may the emergence of an even fitter variant, more transmissible and less lethal. Should this happen, we will be living with this virus for many years—but not necessarily with the disruptive effects of 2020.